Specific Abnormalities
Abnormal scan results? We make sure you are fully informed
Nobody wants to be told they have a heart condition; we believe a more complete understanding empowers you to take the next steps.
Understanding your results in detail.
Echo scans are reported according to internationally established guidelines. As a consequence, the scan results contain numerous technical terms, figures and calculations, which can be readily interpreted by Heart Specialists all over the world, but can be confusing for the non-expert. An explanation of the key anatomical terms and scan findings follows below.
If you need further information on specific cardiac abnormalities, you can find it here.
Search for answers here:
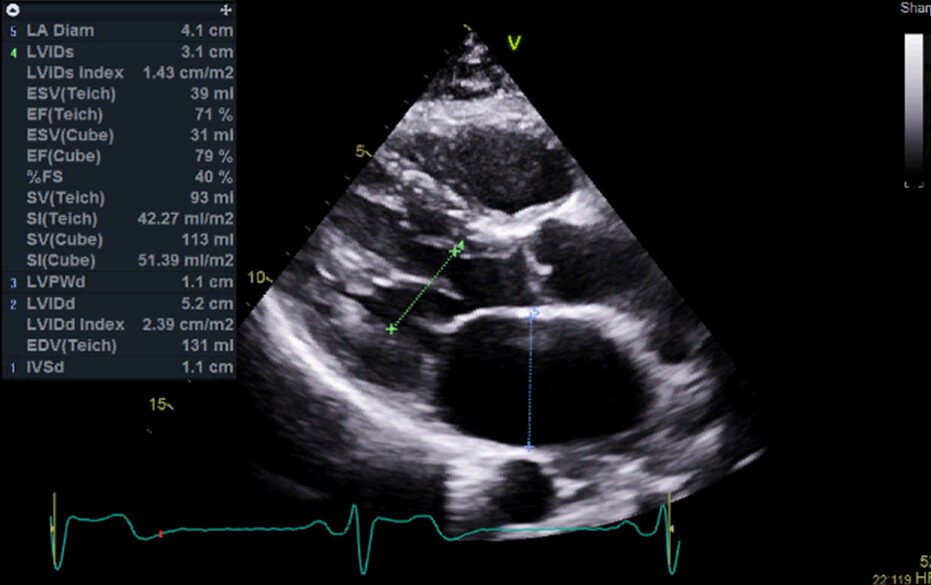
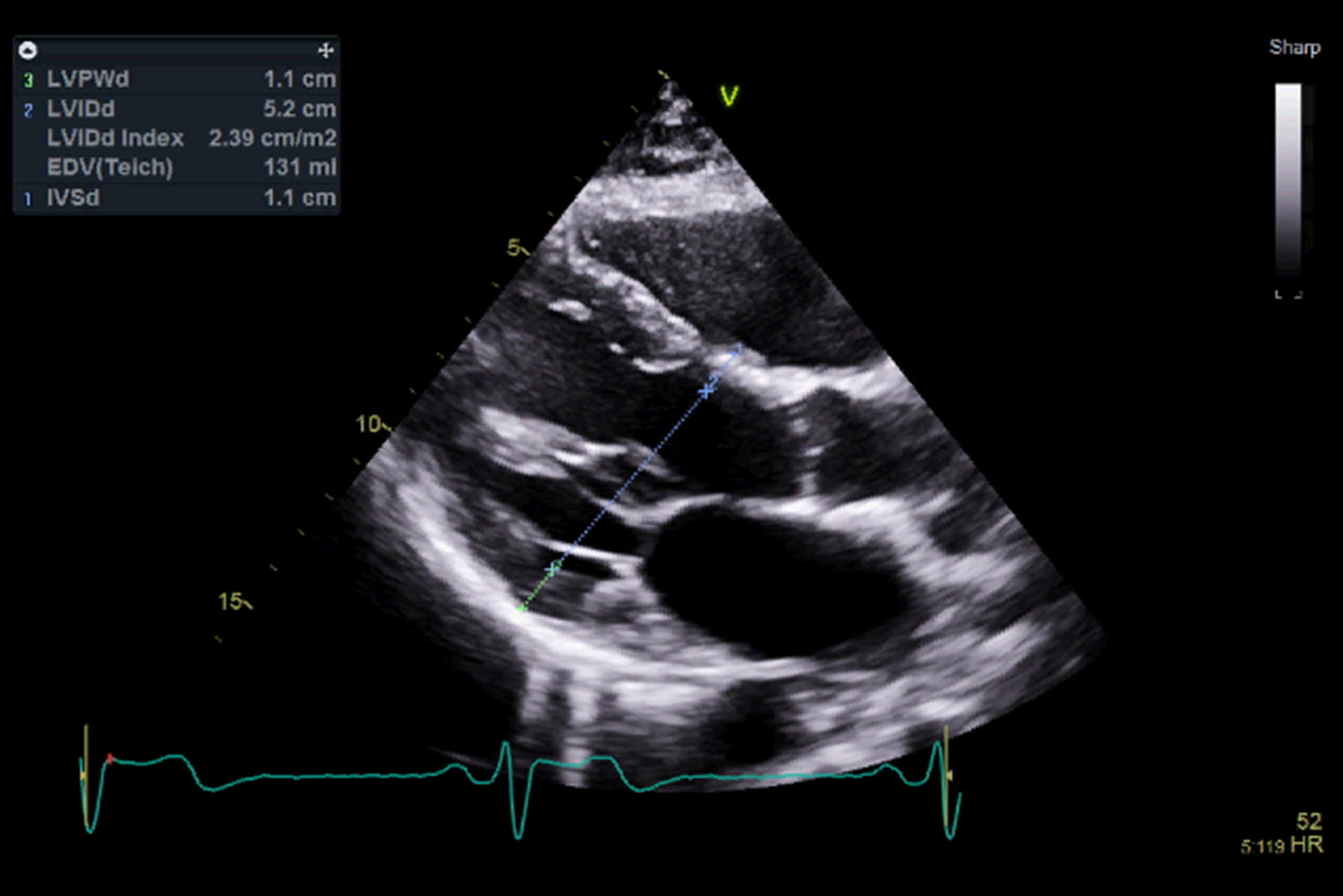
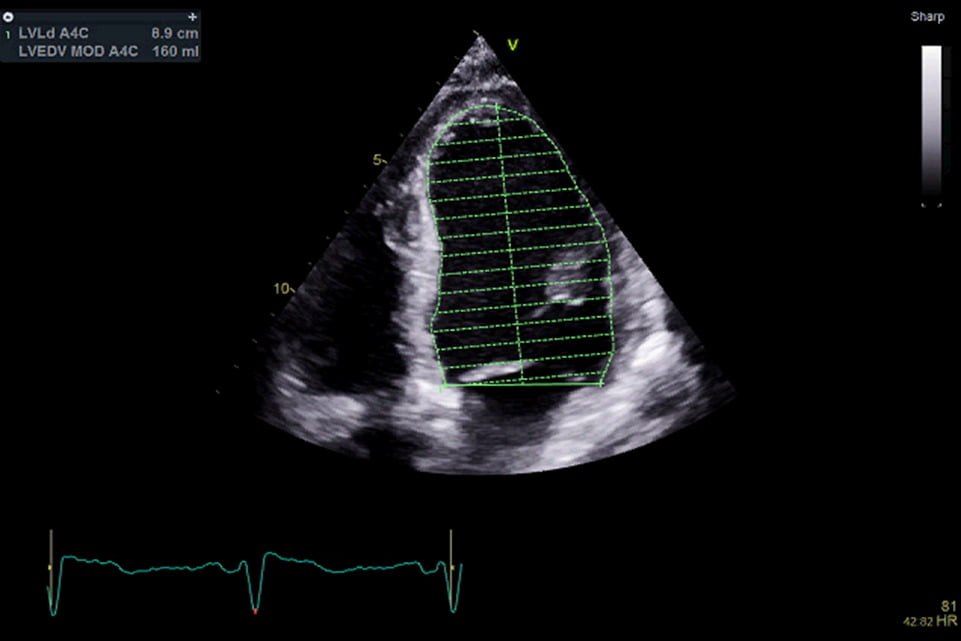
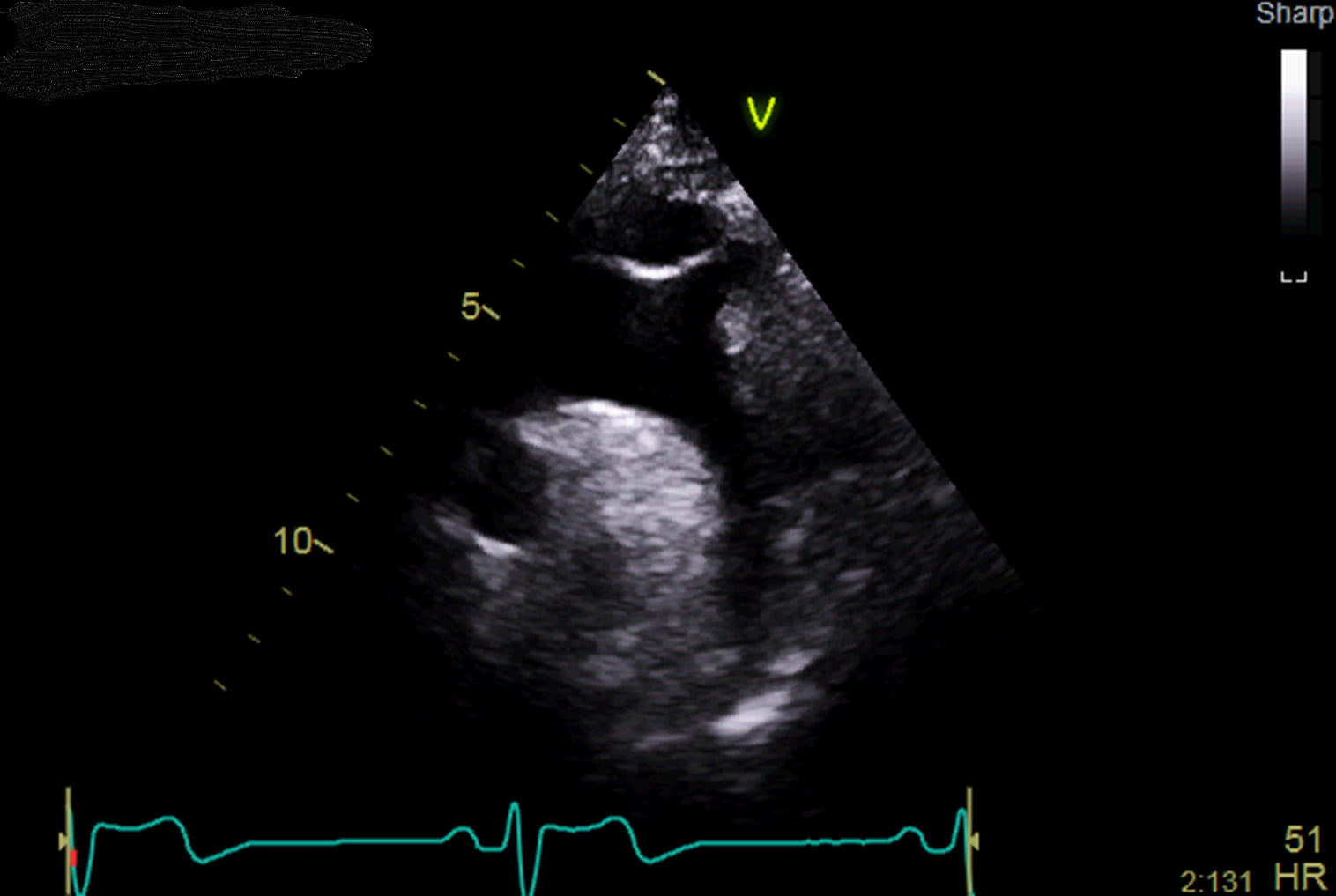
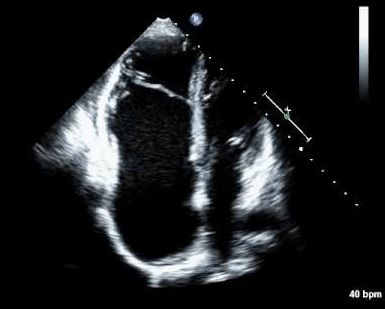
The ventricles – small ventricles can be a normal finding, but occasionally reflect a thickened heart muscle (see below) which leads to an abnormally small chamber. Mildly enlarged (‘dilated’) ventricles can be a normal finding in athletes, but usually reflect early adaptation of the heart’s pumping chambers to another problem, such as a leaky valve. Severely dilated ventricles can be suggestive of heart muscle disease known as ‘dilated cardiomyopathy’ – this diagnosis will require follow-up with a specialist, particularly as the condition runs in families.
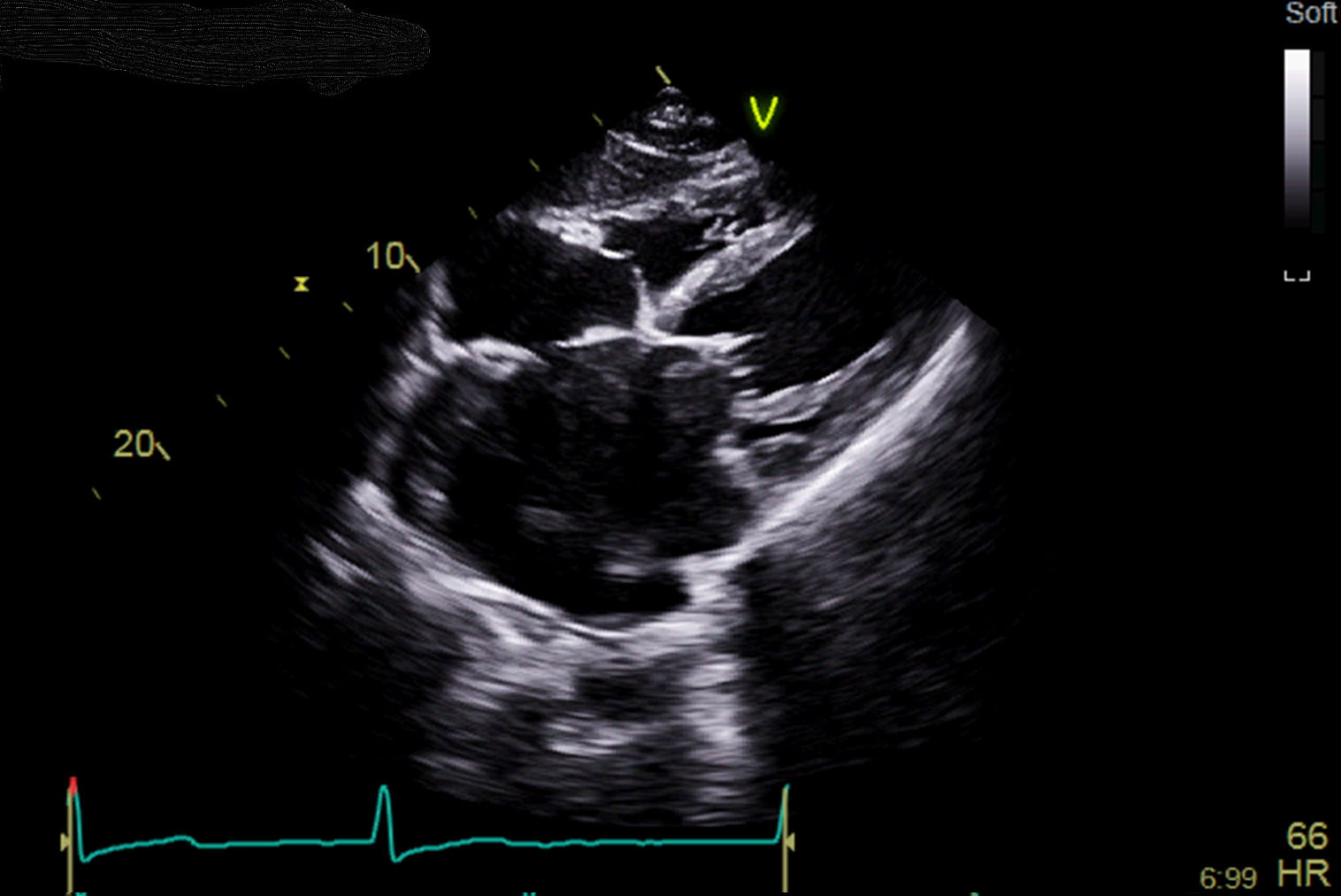
The atria – enlarged atria suggest adaptation of the heart’s filling chambers to another abnormality, such as a leaky valve. For example, mitral valve problems can cause severe dilatation of the left atrium; this dilatation itself does not require specific treatment, however the underlying cause may need referral on to a specialist, and large atria can predispose patients to abnormal heart rhythms.
Thin walls – if the heart muscle is found to be abnormally thin in places, this usually suggests the presence of scar. A scar in the heart can be caused by a number of disease process, such as a previous heart attack or severe infection, and can be a hallmark of certain heart muscle diseases (i.e. a form of cardiomyopathy).
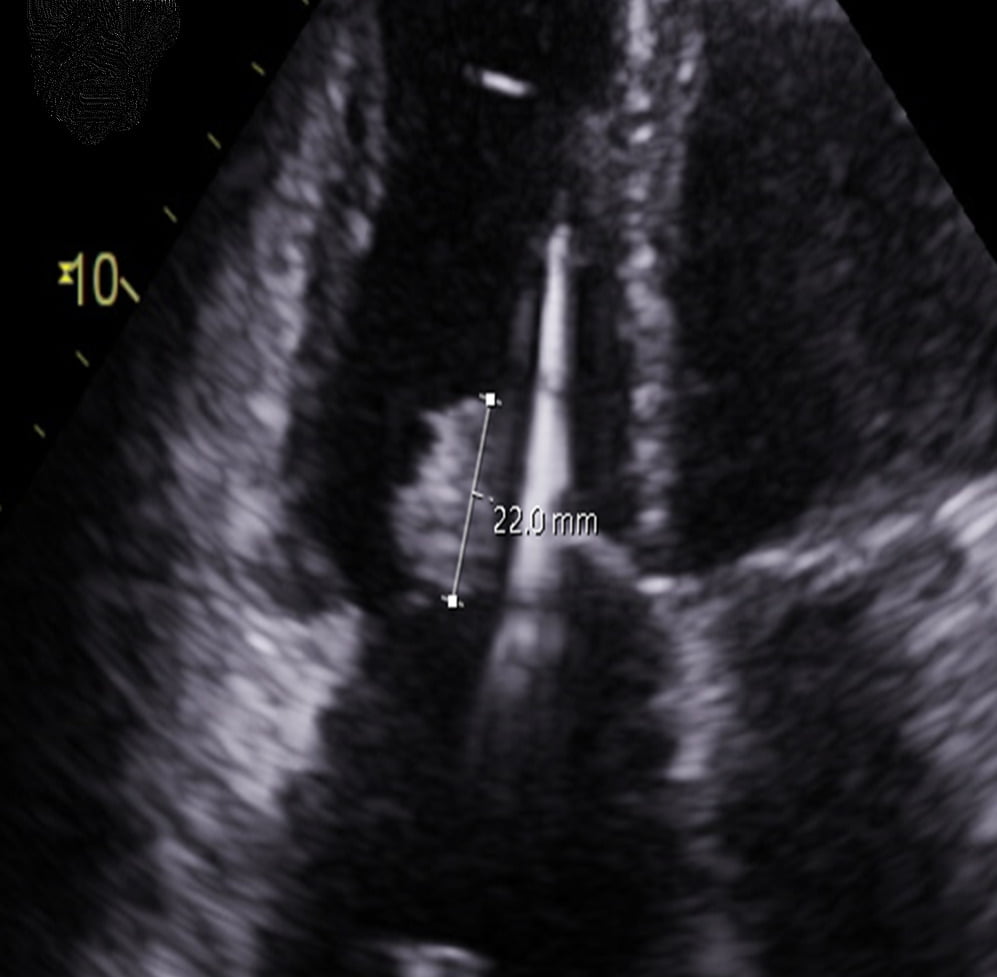
Thick walls – if the heart is forced to pump against increased resistance (such as in cases of high blood pressure or a narrow aortic valve) then, over time, the whole muscle may become thicker to compensate. Global thickening of the muscle is known as ‘concentric hypertrophy’; the management of this involves identification and treatment of the underlying cause. If only a specific area of the heart muscle is thickened (for example ‘asymmetrical septal hypertrophy’), this can suggest a heart muscle disease – namely hypertrophic cardiomyopathy – which will require specialist follow-up.
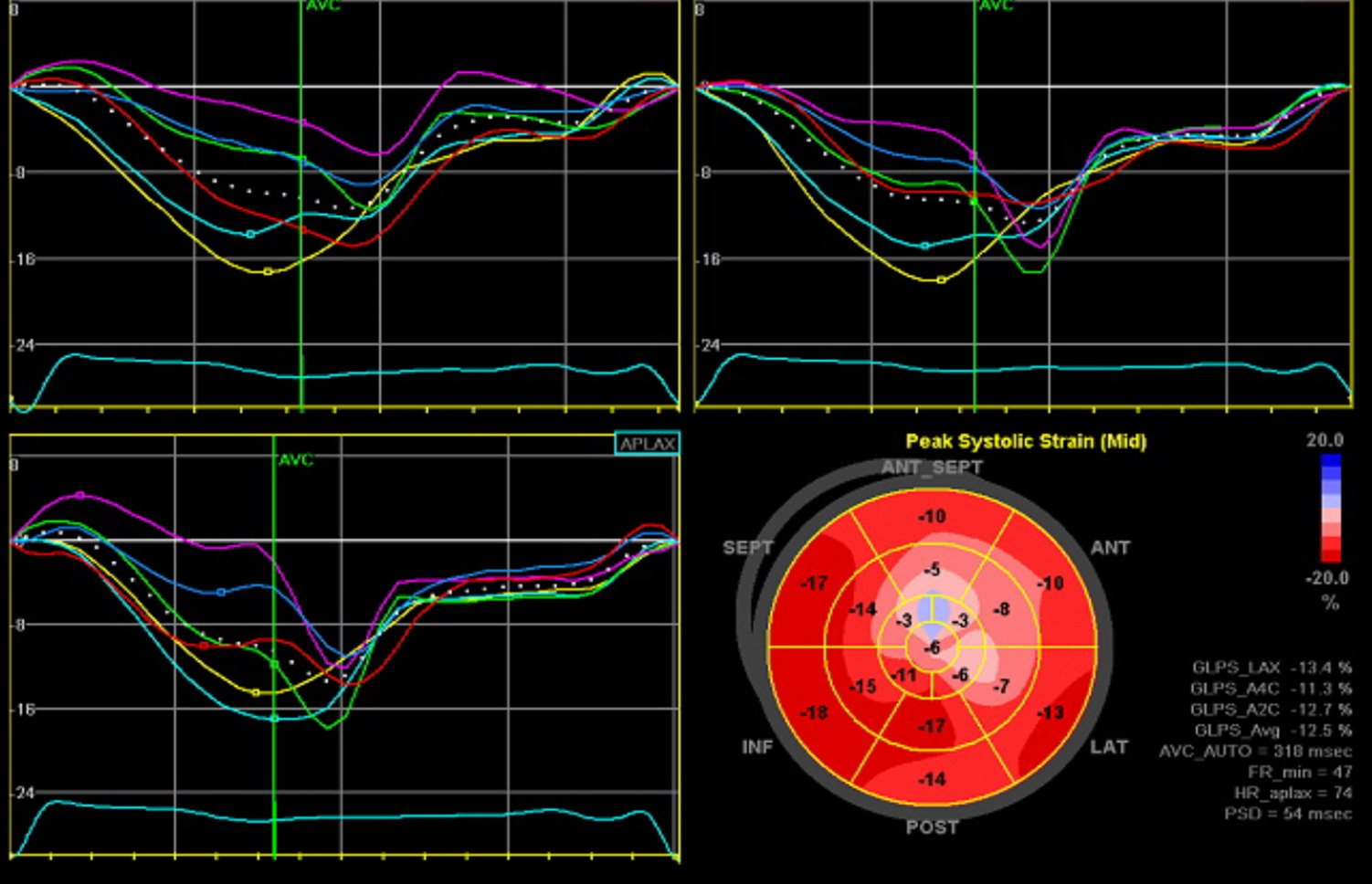
At rest, when the left ventricle pumps (known as ‘systole’), it should empty about 55% of its blood content through the aortic valve and around the rest of the body. This percentage is the ‘left ventricular ejection fraction (LVEF)’, and it is the most useful measure of systolic function. Systolic function is classified as follows:
- LVEF >55% - normal systolic function
- LVEF 50-55% - borderline (or low-normal) systolic function:
- This is often a normal finding, and is particularly common in athletic hearts which, over time, may have adapted and enlarged in response to repeated strenuous exercise. As a result, at rest, athletic hearts may not need to pump as forcefully as non-athletic hearts, and hence their ejection fraction may be slightly reduced
- Our sonographers may sometimes refer to any LVEF >50% as ‘preserved’ i.e. not reduced, which is a reassuring finding
- LVEF 45-50% - mildly impaired systolic function
- LVEF 35-45% - moderately impaired systolic function
- LVEF <35% - severely impaired systolic function
- LVEF >70% - hyperdynamic (i.e. higher than normal) systolic function
Almost all abnormal heart conditions, if left untreated long enough, can cause a reduction in systolic function. The most common symptoms are shortness of breath, fatigue, and ankle swelling. Sometimes, the cause of the systolic impairment is very obvious on an echo (for example, a severe valve abnormality or an inherited heart muscle condition such as dilated cardiomyopathy). However, occasionally the cause is not always clear from an ultrasound alone (for example, we cannot directly visualise coronary artery disease or certain rare inflammatory disorders of the heart), and you will need to be referred for further tests via your GP. All patients with significant systolic impairment will be contacted by our Medical Director to discuss the next steps, which will usually include referral on to your local Cardiologist through your GP. The necessary treatments to try and improve systolic impairment depend on the underlying cause, but include measures to improve the blood flow to the heart, medications, lifestyle changes and, in some cases, implantable devices.
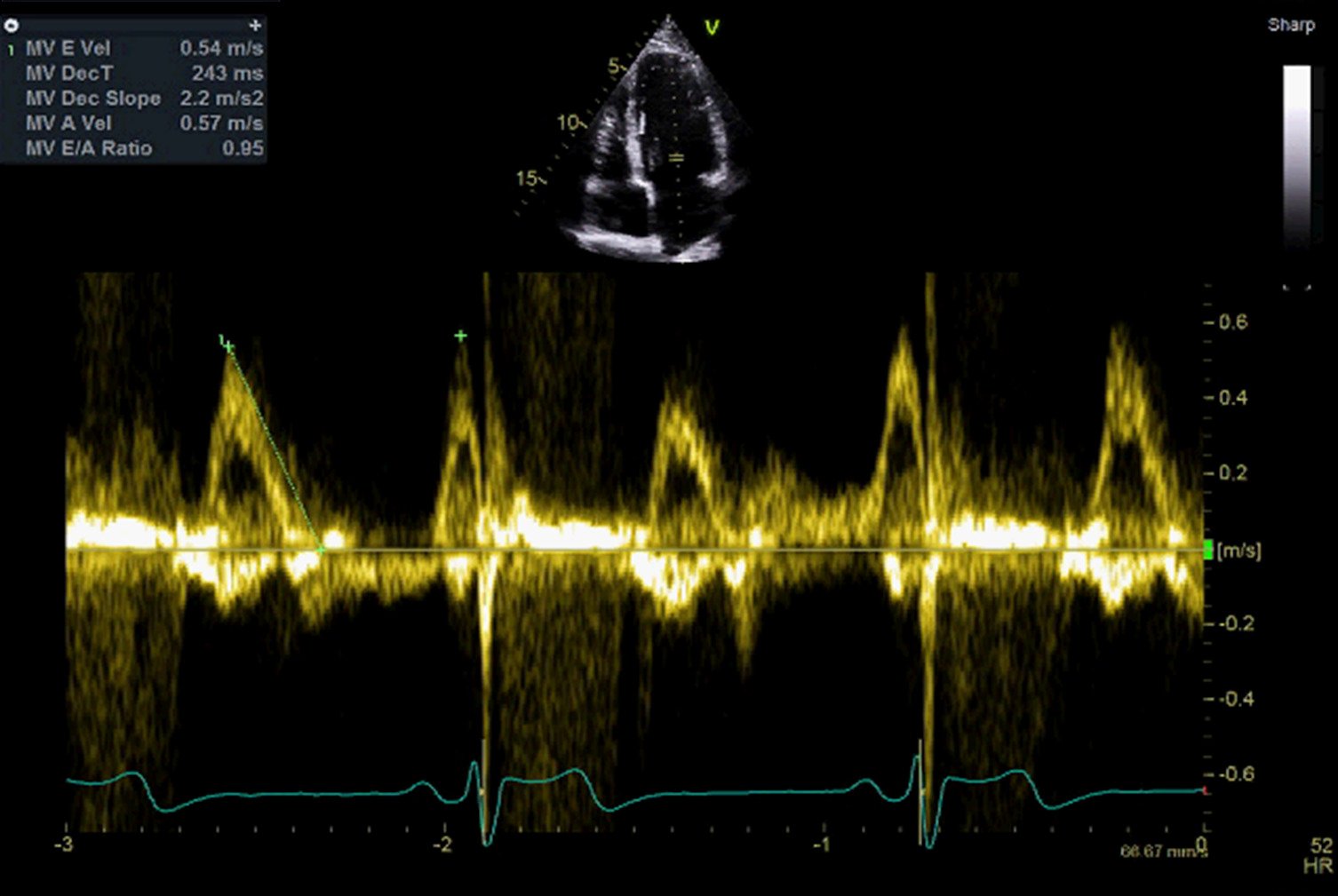
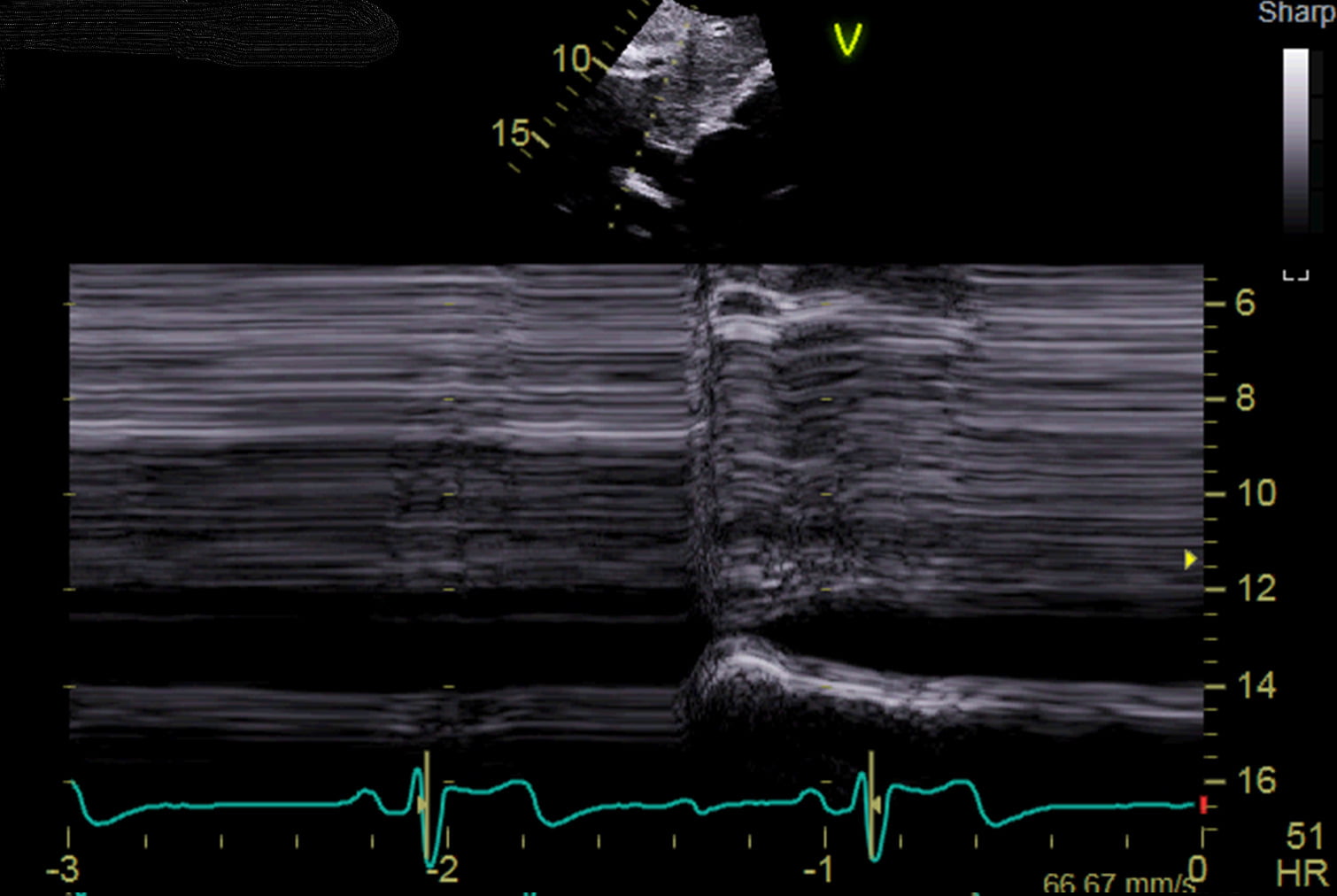
Between contractions, the heart’s ventricles relax (known as ‘diastole’) and fill with blood which has been pumped through from the atria. An echo scan measures the manner and speed with which the ventricles fill – this is ‘diastolic function’. Diastolic dysfunction suggests that there is increased resistance (or stiffening) within the ventricles, and is measured in severity from grades I-IV. Grade I diastolic dysfunction is a very minor abnormality, and is often an expected finding in older people. Grade IV diastolic function (sometimes called ‘restrictive physiology’) suggests a very stiff heart; this can be caused by a number of conditions (such as high blood pressure or coronary artery disease) and may need further investigation, particularly if it is causing symptoms.
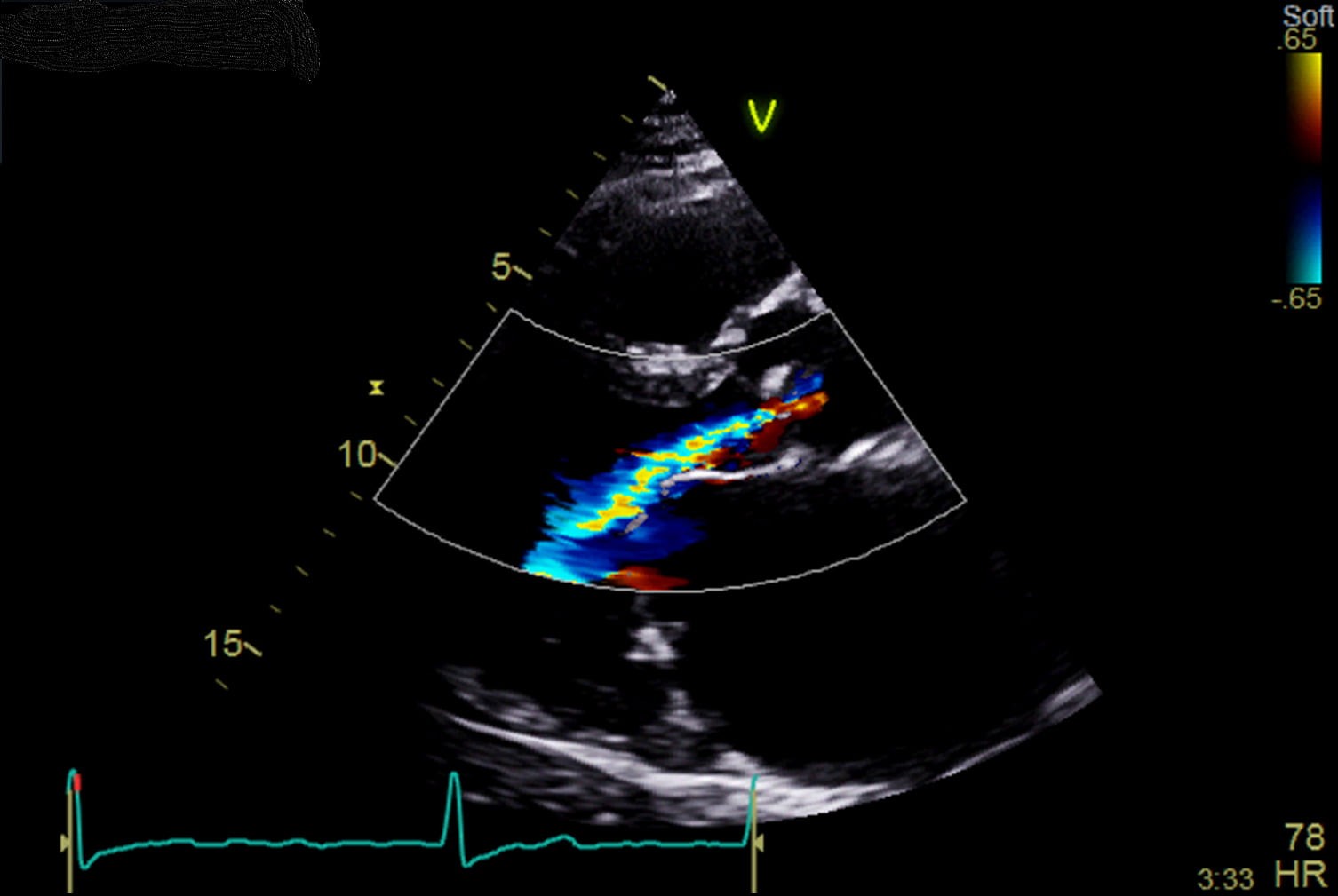
Regurgitation (or a leak) through a valve suggests that the valve either doesn’t close properly, or that it is under increased pressure. For example, patients with lung disease may have high blood pressure in their lungs (known as ‘pulmonary hypertension’), which can put stress on the pulmonary and tricuspid valves, leading to regurgitation when these valves close. Likewise, valves which are abnormally formed or have developed a structural problem (e.g. mitral valve prolapse), will also leak when they close, even if the pressure in the heart is normal. As mentioned above, the degree of valvular regurgitation ranges from trace or trivial (this is a normal finding), to mild, moderate or severe. Whilst our sonographers will be able to give you a visual approximation of any regurgitation on conclusion of your scan, the precise quantification of regurgitation requires detailed calculations and image processing, which take place in the hours following your test. As such, your draft scan report may suggest that one of your valves has moderate regurgitation on visual inspection, and yet – after detailed analysis – your final report may clarify that the regurgitation is in fact only mild, and vice versa.
Mild regurgitation is often in keeping with the normal ‘wear and tear’ of the heart, and may not necessarily progress to a more serious problem. Moderate regurgitation – especially of the aortic or mitral valves – needs careful observation (we are happy to provide this service however follow-up scans may also be available through the NHS). Severe regurgitation is likely to cause unpleasant symptoms, and needs referral to a specialist for further investigation and, if necessary, valve replacement.
Eccentric regurgitation, in which the leak through the valve is at an acute angle, suggests a structural problem in the valve causing abnormal closure (e.g. mitral valve prolapse). Eccentric regurgitation can be difficult to quantify even following detailed analysis, and if it is causing symptoms, this may require specialist follow-up for consideration of an internal echo scan (a transoesophageal echo).
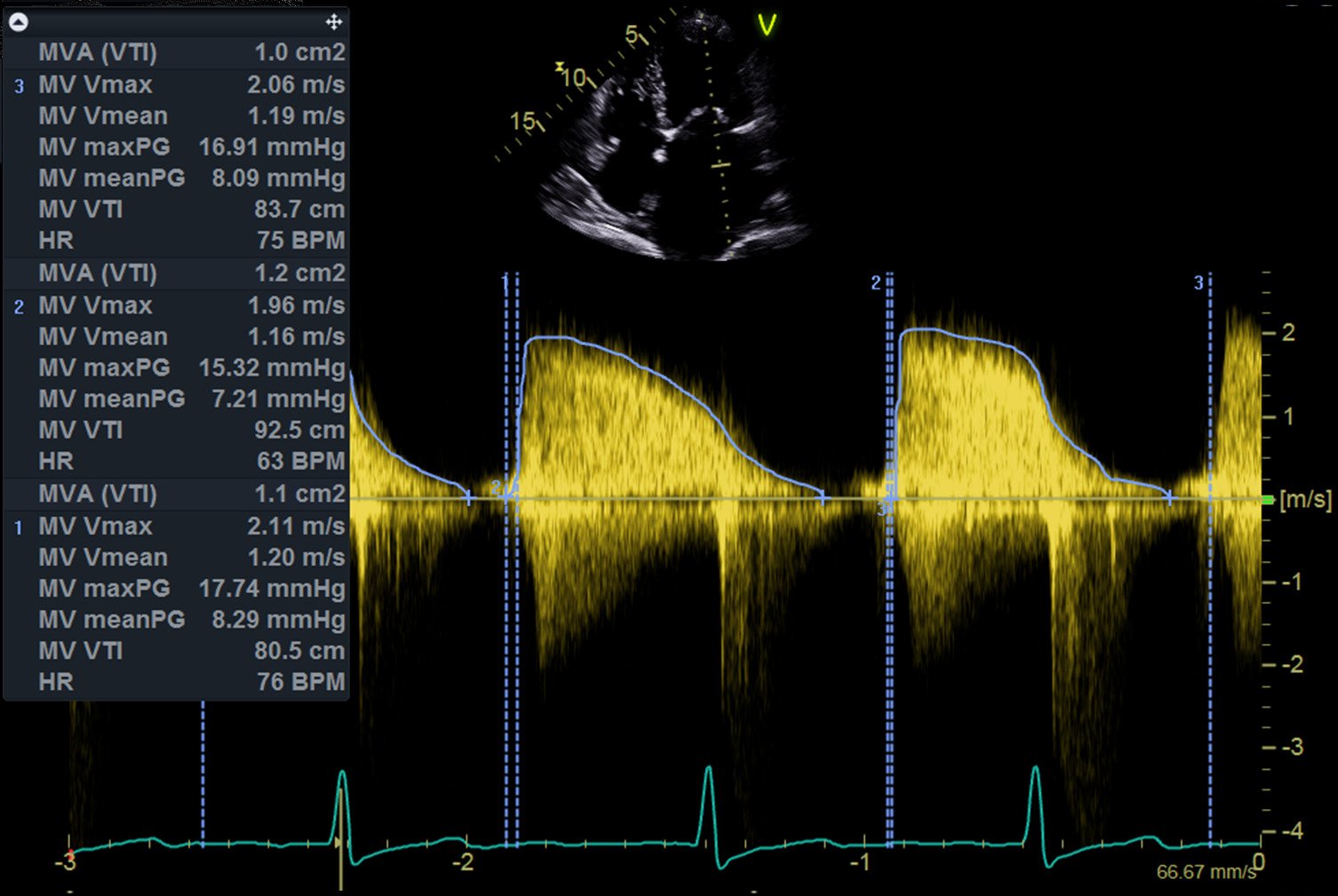
‘Stenosis’ suggests that a valve is abnormally stiff and therefore doesn’t open properly. The most common cause of stenosis is the buildup of calcium on a valve over time (similar to limescale) as people age. Many valves affected by calcification will still open fairly well and are therefore unlikely to cause symptoms (we call these ‘sclerotic’ valves). However, if a valve becomes severely stenosed, this will obstruct the flow of blood out of one of the heart’s chambers, which can cause shortness of breath, chest pain, and even fainting. These valves are likely to need replacing.
Some abnormally formed valves (such as a ‘bicuspid aortic valve’) are predisposed to developing stenosis; these need careful monitoring in specialist clinics.
The left ventricle pumps blood through the aortic valve and into the aorta, which is the body’s largest artery. An echo scan can assess the size of and blood flow through the early part of the aorta. A number of conditions – such as high blood pressure or aortic valve problems – can cause the aorta to enlarge (or ‘dilate’) over time. A mildly dilated aorta is often seen in older people, or people with high blood pressure, and may not cause significant problems, however a severely dilated aorta will need specialist follow-up, and may ultimately need an operation to repair or replace this important blood vessel.
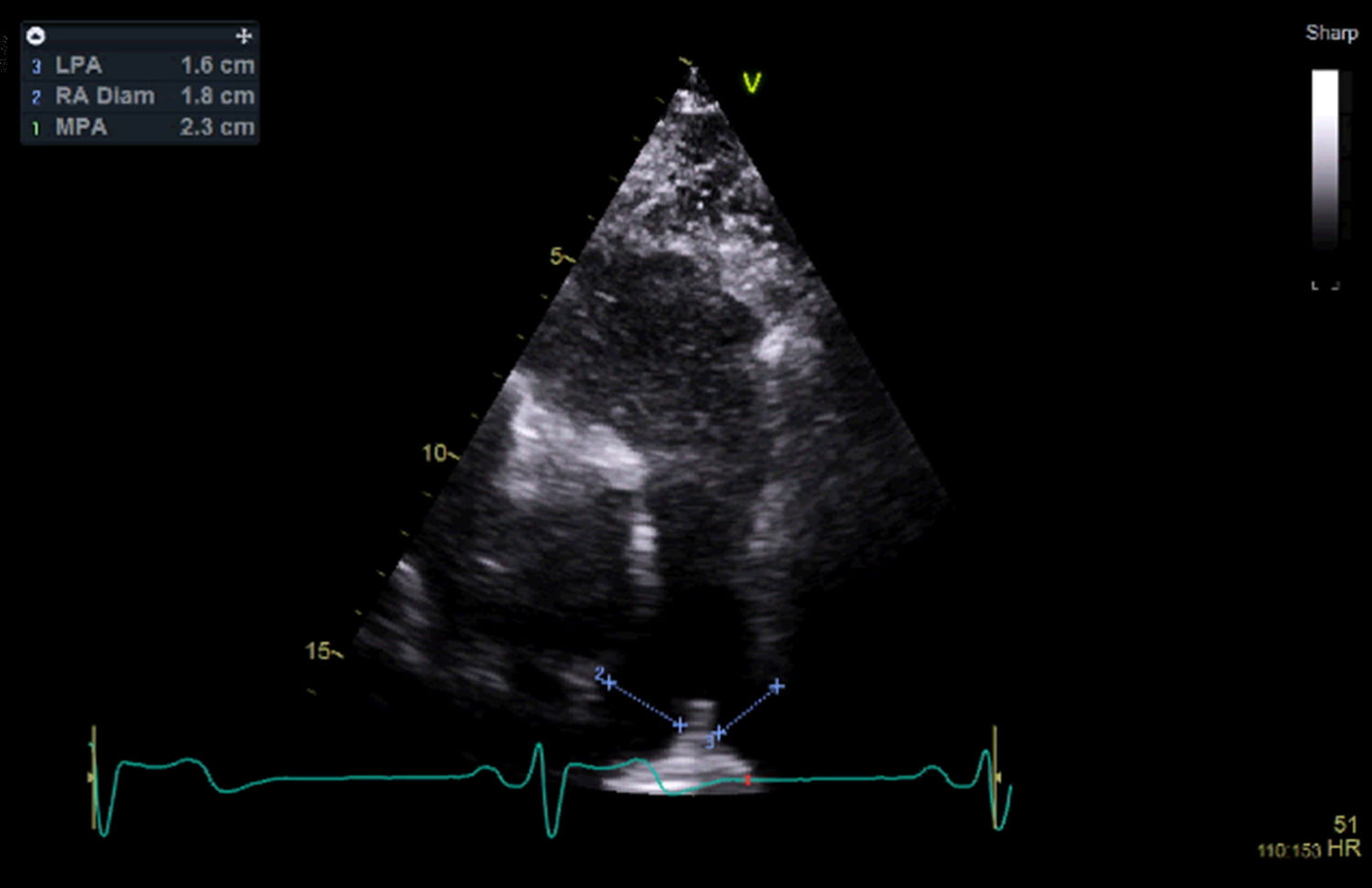
The right ventricle pumps blood through the pulmonary valve and into the main pulmonary artery. This artery subsequently divides into the left and right pulmonary arteries, which collect oxygen from the lungs. By examining the size of and flow through the pulmonary arteries, we can estimate the blood pressure within the lungs. In addition, because raised pressure in the lungs puts the right ventricle under strain, this will often cause a leak (regurgitation) through the tricuspid valve. If we measure the severity of this leak, we can also calculate an approximation of the blood pressure in the lungs (often documented in a scan report as PA(S)P – pulmonary artery (systolic) pressure – or RVSP – right ventricular systolic pressure). Raised blood pressure within the lungs is known as pulmonary hypertension; this is most often caused by lung disease (such as COPD), or by a buildup of pressure further downstream, such as a valve problem in the left side of the heart. However, there are some more uncommon causes of pulmonary hypertension which, if severe, may need further investigation and treatment.
The vena cava is the largest vein in the body, and it collects and drains blood back into the right atrium. The IVC may be dilated in any condition which raises the pressure within the heart, such as a leaky valve.
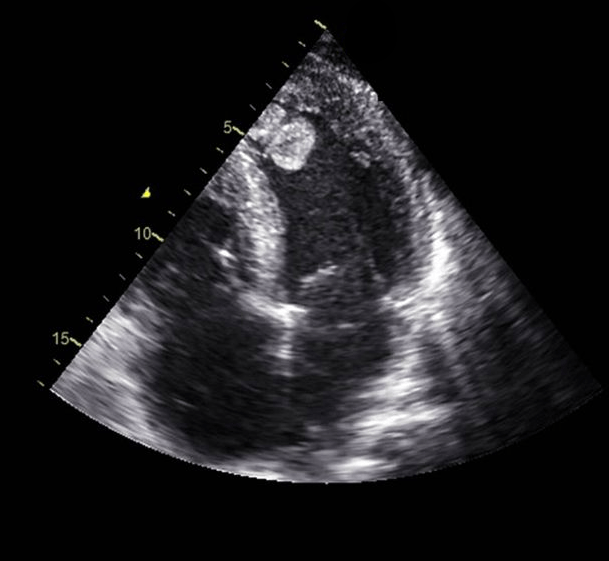
The pericardium is the sac which lines the outside of the heart. It is normal for the pericardium to contain a small amount of lubricating fluid. A more significant collection of fluid is known as a ‘pericardial effusion’, this can be a normal finding, but is occasionally a sign of a multi-system disease, such as an autoimmune condition. A large pericardial effusion will require further investigation and, if it is restricting the filling of the heart, will require drainage by a specialist.
Very rarely, echo scans find abnormal masses in the pericardium. If the mass is suspicious for a tumour, we will refer you urgently for specialist investigation.
A number of abnormal structures can be seen attached to the heart valves. An infected heart valve may develop a visible collection of bacteria known as a ‘vegetation’; however, most of these patients will have reported severe symptoms – such as fevers and breathlessness – before their scan has been performed, and hence vegetations are usually discovered in the hospital setting. In addition, there are some benign tumours – such as ‘Lambl’s excrescences’ or ‘fibroelastomas’ – which can grow on valves and, depending on their size and associated symptoms, may need referral for removal.
Primary cardiac tumours – such as a left atrial ‘myxoma’ – are extremely rare. If your scan is suspicious for a tumour, you will be referred for specialist investigation.
A blood clot – or ‘thrombus’ – is an unusual finding in the heart, but can be encountered in patients with a recent heart attack, or in cases of very severely reduced systolic function. These cases will need referral for consideration of blood thinning medication. Very small blood clots can be difficult to see on a standard cardiac ultrasound; if there is any doubt, you may be referred for consideration of an alternative imaging test.
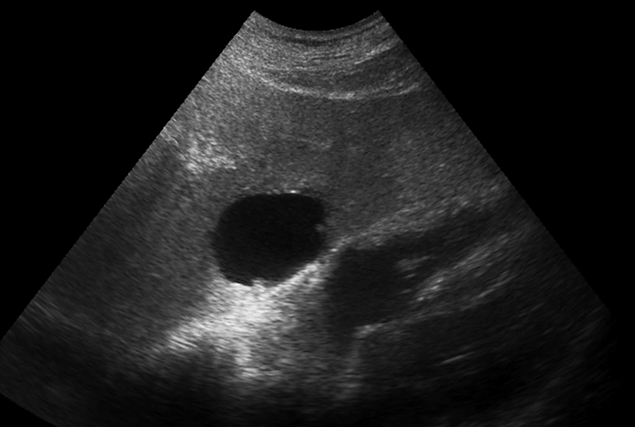
In the process of performing an ultrasound of the heart, we occasionally see abnormalities in the lungs (such as fluid) or the liver, which may require referral for alternative imaging.
Significant congenital heart abnormalities are usually identified in childhood, but there is a possibility your scan may identify a structural anomaly that you were born with, such as a hole in the heart. This will need referral on to a Congenital Heart Disease specialist for further investigation.
Book Your Heart Scan Today